Inflammatory Bowel Disease Disparities
Inflammatory Bowel Disease is a set of diseases that attack the Intestines. It leads to chronic inflammation in the lining of the digestive tract. If left untreated, IBD can be life-threatening and change the way one lives. Many suspect an immune system malfunction to be the primary cause of Inflammatory Bowel disease along with diet, Environment, and genetics. Crohn's disease and Ulcerative colitis come under Inflammatory bowel disease and are very similar. Although there is no cure for these diseases, many people may experience remission.
It has been thought that IBD presents mainly in Caucasians. However, more data has been proven that people with different ethnic groups are being affected more. During a 2014 study, out of 10,000 people, about ten people of Hispanic descent, 25 Black people, and 70 non-Hispanic people will get IBD.
Many studies also report that minority populations tend to be underrecognized, which may hinder the process of coming to a diagnosis. If waited too long, inflammation can get out of hand and lead to cancer, fistulas, and strictures in the bowel.
According to another study, African American Crohn's disease patients are less likely to be in remission, are more likely to have surgery, and are more likely to have post-surgical complications. Lower income is connected to a greater risk of severe illness, IBD-related hospitalizations, ICU stays, and mortality, among other things. It is essential to work together and to be heard. IBD is not a well-known disease; you can spread knowledge from person to person so they understand the severity of this disease. Every small step makes a substantial difference in the greater run.
By: Samhita Di
What is Healing?
At first glance, the word healing in the context of healthcare may seem to be curing an illness, helping someone else get healthier, or even easing symptoms of a disease. However, the field of medicine doesn’t have an operational definition of healing. Although medicine is considered a healing profession, it places more emphasis on the physiological mechanisms of curing patients.
According to “The Meaning of Healing: Transcending Suffering”, healing may be operationally defined as the personal experience of the transcendence of suffering. Physicians can enhance their abilities as healers by recognizing, diagnosing, minimizing, and relieving suffering, as well as helping patients transcend suffering (Source). This means that physicians can help patients who view suffering as an opportunity for affirming spiritual values and see suffering as a spiritual test (Source).
Healing has also been associated with wholeness, narrative, and spirituality. It has been described as “an intensely personal, subjective experience involving a reconciliation of the meaning an individual ascribes to distressing events with his or her perception of wholeness as a person (Source).”
The increasing values of empiricism and Cartesian reductionism in Western medicine have certainly brought upon many advances in science and treating ill patients. Yet, these advances came at the price of healing an ill patient, particularly when there is no physical cure for a chronically ill patient. However, throughout history, spirituality and health have been intertwined. In many present day Western hospitals that were founded by religious orders and organizations, one can almost always find a chapel present. Priests recite morning and night prayers over the intercom. A cross can be found in every room of the hospital. Many religious texts offer definitions for health and healing, the most prominent being the Bible in both the Old and New Testaments.
Even though curing and healing may appear to be very similar, the difference between the two can be summarized through a quote by Susan Howitch from Absolute Truths: “A cure signified the banishment of physical illness, but a healing could mean not just a physical cure, but a repairing and strengthening of the mind and spirit to improve the quality of life even when no physical cure was possible.” Such spiritual care can be found in palliative care and hospice care in which the relief from suffering is prioritized for patients who are experiencing chronic illnesses.
By: Sreenidhi Saripalli
Celebrate Thanksgiving in a Culturally Appropriate Way!
Happy Thanksgiving to our readers at Humanity In Health! We are so thankful for each and every one of you for taking the time to learn more about cultural competency as a future healthcare professional and working towards eliminating disparities!
Over the years Thanksgiving has become a great way to get together with families and enjoy meals while taking the time to be grateful for each aspect of our lives. However, we must always keep the history behind this holiday in the back of our minds and remember the many Native Americans who were forced to give up their lands to colonizers. Thus, we must make every effort to celebrate this classical holiday in a culturally appropriate way.
First, we can recognize other typical thanksgiving traditions that happen elsewhere. “How to celebrate Thanksgiving in a Culturally Appropriate Way” mentions many other Thanksgiving celebrations such as the British Harvest Festival, a Jewish harvest festival Sukkot, Christian harvest from Germany, and the Japanese holiday for Labor Thanksgiving Day which originates from the Shinto harvest ceremony (Source). By celebrating other cultures and traditions, we can stray from the insensitivity of American Thanksgiving’s history and expand our celebrations.
Next, we must also learn about the start of American Thanksgiving that began when British settlers came to America. With the help of the Native Americans, the settlers were able to successfully produce a harvest that could feed themselves. To celebrate their achievement, the settlers threw a large feast and invited many of the Native American allies. Although this story seems like a joyous celebration, in reality, there was and still is a long history of injustice towards the Native Americans who first inhabited America (Source).
Finally, we can listen to the Native American voices of our country. The Wampanoag People were the first to assist the Pilgrims when they arrived from Europe. Their generosity was truly taken advantage of and its reality has been largely skewed. But, we can all listen to the cultural context and implications of Thanksgiving in an interview with Cedric Cromwell, the Tribal Council Chairman of the Mashpee Wampanoag Tribal Nation. (Source).
By: Sreenidhi Saripalli
Because Mental Health X Humanity In Health: Mental Health Awareness
Hi! My name is Sree Saripalli and I’m the founder of Humanity In Health. In honor of collaborating with Because Mental Health, I’m going to be talking about mental health awareness in today’s blog post.
My first experience learning about mental health was quite a positive one. I remember learning about the different mental challenges people face when I was in around 6th or 7th grade through a school seminar that covered topics such as anxiety, depression, PTSD, and many more. Openness, acceptance, and compassion were highly encouraged, and I left the seminar feeling like someone had shown me a completely different side to human health. I was immediately intrigued and wanted to learn more. Through books, movies, and social media, I started to gain a first hand perspective of what it is like to live with a mental disorder or a personality disorder. When I took AP Psychology my junior year of high school, I was able to learn more about these disorders from a scientific view point.
But how exactly do we communicate with those who are struggling with a mental illness?
Below are 8 things to do that support someone with a mental illness outlined by Mental Health Foundation:
Set time aside with no distractions
Let them share as much or as little as they want
Don’t try to diagnose or second guess their feelings
Keep questions open ended
Talk about well being
Listen carefully to what they tell you
Offer them help in seeking professional support and provide information on ways to do this
Know your limits
A more detailed explanation of the 8 things to do can be found on the Mental Health Foundation website linked here: https://www.mentalhealth.org.uk/publications/supporting-someone-mental-health-problem
While it can be helpful to know what to do when communicating with someone facing mental health challenges, it is important to conversely know what NOT to say. Aruma provides a comprehensive “10 things not to say to someone with a mental illness” list outlined below.
“It’s all in your head”
“Come on, things could be worse!”
“Snap out of it!”
“But you have a great life, you always seem so happy!”
“Have you tried chamomile tea?”
“Everyone is a little down/moody/OCD sometimes - it's totally normal.”
“This too shall pass.”
“It’s all part of God’s plan.”
“Just try to be positive!”
“Suicide is so selfish.”
A more detailed explanation of the list can be found here: https://www.aruma.com.au/about-us/blog/10-things-not-to-say-to-someone-with-a-mental-illness/
When someone has a fever, we can measure their temperature. With a cold, we see them cough or sneeze. When someone has a broken arm, we can perform surgery and we see the cast. We may even sign it to show our support! However, mental health is a unique aspect of health that is not always so easily visible. It can be hard to demonstrate cultural competence, empathy, and clear communication when addressing such situations. Hopefully, this article helps you or a friend in need!
By: Sreenidhi Saripalli
Medical Sociology
From discussing medical practices in other religions, exploring how social determinants affect health care, exploring different philosophies in medicine, to learning about various medical disparities, Humanity In Health seems to cover a wide span of topics. But what exactly is all of this information? Although all of this may not seem like it would make a direct impact on the healthcare industry, medical sociology, the study of social causes and consequences of health and illness (source), affects large populations. In today’s blog post, we will be going over what medical sociology is, why it is so important, and how we can pursue it at a higher level.
Medical sociology may very well seem to be an abstract topic at first glance. However, it has vast implications in the field of health care and is an integral part of the medical system. According to the American Sociological Association, medical sociology “provides an analytical framework for understanding the social contexts of health, illness and health care. Central topics include the subjective experience of health and illness, political, economic and environmental circumstances fostering ill health; and societal forces constraining the medical care system and individuals' responses to illness. This field draws on traditional sociological issues and contributes to them through reformulations of such basic concepts as social systems and institutions, professionalism, social movements and social change, and social interaction and negotiation. Drawing from pluralistic perspectives, the field is concerned with basic sociological research and its implications for public policy and practice.” The range of topics covered by medical sociology can include specific cultures’ health policies and practices, religious differences in approaches to medicine, and disparities faced by certain ethnic groups.
Although medical sociology isn’t typically what first comes to mind when one mentions healthcare, it is undeniably a vital component of the healthcare field. Medical sociology strives to understand why certain patterns occur in healthcare and what we can do as either patients or providers to help the healthcare experience be the best it can be. As the diversity of many countries increases, it becomes more important to become aware of differences among ethnicities, races, and certain populations when it comes to availability and approach to healthcare. This knowledge helps us gain awareness when interacting with people, patients, or providers who might not come from the same background as us.
Most medical sociologists start off as sociology majors in their undergraduate years. From there, they specialize in the medical side of sociology. Job opportunities for medical sociologists include community health workers, nurses, psychologists, hospital administrators, policy analysts, and human resource representatives. Medical sociologists can impact the way healthcare facilities are able to care for their patients using their extensive knowledge. Additionally, those who obtain masters and doctorates can become social health scientists. These individuals can become professors, publish books, and research new policies for the healthcare operating system (source).
By: Sreenidhi Saripalli
Elizabeth Blackwell: Champion of Gender Equality in Healthcare
Nearly 70% of the global healthcare workforce today is comprised of women, with over 75% of US healthcare jobs being held by women (source). But how did that happen in what has been a largely male-dominated society for centuries? In today’s blog post, we will explore the life and legacy of Elizabeth Blackwell, the first woman to receive a medical degree in the United States and a champion for women’s rights in healthcare.
Elizabeth Blackwell was born in England on February 3, 1821. She was one of nine children born to an anti-slavery activist and had famous relatives, including an abolitionist and a women’s rights activist (source). Perhaps this is what encouraged her to advocate for equality in healthcare!
In her book, Pioneer Work in Opening the Medical Profession to Women (1895), Blackwell wrote that her inspiration to pursue medicine came after a dying friend said having a female physician would have alleviated her suffering. She consulted several physicians for advice on pursuing a career in medicine, but all of them told her it was impossible, as it was expensive and medical education was not available to women. However, Blackwell accepted the challenge and applied to all the medical colleges in New York and Philadelphia. She was rejected to all but one: Geneva Medical College in New York. The faculty allowed the all-male student body to vote on her admission. As a joke, they all voted yes, allowing her to gain admittance (source).
During her time in college, Elizabeth Blackwell faced much discrimination and overcame many obstacles. For example, her professors forced her to sit separately and locals rejected her for defying her gender role. In 1849, she became the first woman to receive a medical degree from an American school, finally earning her the respect of her classmates and teachers!
Blackwell continued training in London and Paris hospitals, where she studied midwifery and emphasized preventative care, calling out male doctors for not washing their hands in between patients. In 1851, after losing sight in one eye, she returned to New York City, where she had few opportunities due to discrimination against female physicians. In 1857, along with her sister and colleague, Elizabeth Blackwell opened the New York Infirmary for Women and Children, which provided training for women physicians. A decade later, in 1868, Blackwell opened the Woman’s Medical College in New York. This was done in collaboration with Florence Nightingale, another pioneering woman in healthcare! (source).
In the 1870s, as her health began worsening, she gave up the practice of medicine, but never stopped campaigning for reform (source). Elizabeth Blackwell’s passion for medicine and persistence in her fight for equality allowed her to overcome the depths of adversity. Today, she is recognized by medical professionals globally and the legacy she left behind continues to inspire young girls and women around the world.
By: Sailee Naik
Editor: Sreenidhi Saripalli
Gender Bias In Healthcare
16 year old Jackie was suffering from chronic kidney problems, fevers, fatigue, and menstrual and joint pain. After numerous visits to a primary care doctor, urologist, and pulmonologist, Jackie was dismissed as simply having depression due to a lack of results from tests pointing out anything amiss. Years later, Jackie was finally able to attribute her symptoms to endometriosis and received the proper treatment (source).
Unfortunately, the initial stages of Jackie’s situation are more common than one might expect. Hundreds of women who seek the expertise of physicians are told that their symptoms are due to hormones, stress, or they are just “overreacting”, “hormonal”, and “making things up”. This phenomenon is referred to gender bias and stems from implicit bias that follows physicians into the clinic.
Similar to Jackie’s initial diagnosis of depression, many women often get their physical complaints attributed to mental illness. This attribution has roots in the history of the mythical illness “hysteria” that is blamed on a “wandering womb” or sensitive nerves. Eventually, hysteria was seen as a psychological illness in the post-Freud era. Although the terms used to describe hysteria have changed over time, the concept that the unconscious mind can produce physical symptoms has persisted in medicine and has most prominently been acquainted with female patients.
For a long time, women have been seen as the standard patient who has psychological problems. However, due to the diagnosis of psychological problems, physicians are more likely to dismiss physical complaints from women as being “all in their heads”. A study conducted in 1986 looked into a group of patients who had been diagnosed with neurological disorders who had previously been diagnosed with “hysteria”. The group found that such a misdiagnosis was common among women who had been diagnosed with a previous psychological disorder.
The gender bias in healthcare also stems from the belief that men and women only have physical differences when it comes to reproductive organs. Thus, most research was conducted on male animals and male cells. However, advances in science and technology show that there are more significant differences between males and females. Janine Clayton, MD, states that “because we have studied women less, we know less about them. The result is that women may not have always received the most optimal care” (Source).
It can be difficult to address gender bias in healthcare since we are often not aware of the issue. The first step in combating gender bias in healthcare is simply recognizing that this unintentional bias exists. Other steps we can take, as outlined by Duke Health, are encouraging open discussions of gender bias in healthcare and using substitution. Think about how you would address the same patient if they were of a different gender and reflect on the differences between the hypothetical interaction and the patient interaction. Additionally, we can make an effort to ask the patient open ended questions such as “What are your concerns for today?”
As Denise Davis, MD, says, “biases are not moral failings; they are habits of the mind”. With time and effort, these habits can be changed. But we first must acknowledge the seriousness of the gender bias issue in healthcare and make efforts to eliminate it.
By: Sreenidhi Saripalli
Implicit Bias in Healthcare
There are many racial inequities in healthcare. From the numerous disparities to barriers to healthcare, it’s no secret that not everyone has the opportunity to obtain quality healthcare. And while there are numerous causes to explain why these unfortunate events occur, it is important to acknowledge a key concept in patient care and healthcare delivery that contributes to these disparities: implicit bias.
Implicit bias, according to dictionary.com, refers to “the bias that results from the tendency to process information based on unconscious associations and feelings, even when these are contrary to one’s conscious or declared beliefs. The Kirwan Institute for the Study of Race and Ethnicity at Ohio State University states that “implicit bias, also known as implicit social cognition, refers to the attitudes or stereotypes that affect our understanding, actions, and decisions in an unconscious manner. The bias can be positive or negative and is activated involuntarily without an individual’s knowledge or control.”
In the healthcare field, implicit bias can affect the ways in which a healthcare provider communicates with their patient. Since implicit biases are unconscious attitudes, they often seep into communication without the individual realizing it. One example of this is when a healthcare provider makes assumptions about a patient based on the patient’s appearance. This is shown through data from the Regenstrief Institute from the Department of Veterans Affairs when they conducted a survey of 85 Black veterans.
The data suggested that veterans accessing mental health treatment could sense non-verbal cues that suggested implicit bias. The research team quoted a respondent of the survey who stated that they felt stereotyped as “angry, big Black men”. The respondents explained that “some providers viewed them as a physical threat and reacted fearfully”. Other examples of implicit bias in healthcare can include making assumptions about the patient’s behaviors, education levels, socioeconomic status, and other factors that may be associated with their appearance.
It is important that we address our implicit bias early on, since these harmful notions can lead to further healthcare disparities and inequalities. But how do we take action to reduce and eliminate our implicit bias? Very Well Mind outlines 6 simple steps to take in order to achieve this:
Focus on seeing people as individuals: Instead of focusing on stereotypes to define people, spend time considering them on a more personal, individual level.
Work on consciously changing your stereotypes: If you do recognize that your response to a person might be rooted in biases or stereotypes, make an effort to consciously adjust your response.
Take time to pause and reflect: In order to reduce reflexive reactions, take time to reflect on potential biases and replace them with positive examples of the stereotyped group.
Adjust your perspective: Try seeing things from another person's point of view. How would you respond if you were in the same position? What factors might contribute to how a person acts in a particular setting or situation?
Increase your exposure: Spend more time with people of different racial backgrounds. Learn about their culture by attending community events or exhibits.
Practice mindfulness: Try meditation, yoga, or focused breathing to increase mindfulness and become more aware of your thoughts and actions.
Heath, Sara. "What Is Implicit Bias, How Does It Affect Healthcare?"
Patientengagementhit, 16 Oct. 2020, patientengagementhit.com/news/
what-is-implicit-bias-how-does-it-affect-healthcare. Accessed 30 Mar. 2021.
By: Sreenidhi Saripalli
Neglected Diseases
In impoverished areas of the world among populations of lower socioeconomic status, many diseases are often overlooked and inhibit the daily lives of many people. These diseases are known as neglected diseases and affect more than 1 billion people according to the World Health Organization. Neglected diseases are most common in areas of Africa, Latin America, Asia, the Middle East, and parts of the United States where poverty rates are high, drinking water is unsafe, sanitation is poor, housing is substandard, and there is limited access to healthcare.
The reason neglected diseases are called as such is due to the lack of attention given to them by drug developers, government officials, public health programs, and the media. Although the cost of producing drugs for some of these diseases can be low, the people suffering from these diseases often cannot afford to treat the diseases. Thus, private pharmaceutical companies aren’t always able to develop and produce treatments. Additionally, neglected diseases most commonly affect underdeveloped nations, and they aren’t considered high priorities for prevention and treatment. Another reason neglected diseases are overlooked is that they don’t cause dramatic outbreaks. Rather, they take effect over long periods, leading to deformities, disabilities, and relatively slow deaths.
Neglected diseases most typically take the form of tropical diseases that are caused by parasites. Some examples of tropical diseases include African trypanosomiasis. This disease is “commonly called sleeping sickness, and is caused by a parasitic microbe transmitted by tsetse flies. If untreated, the parasite migrates to the central nervous system, causing seizures, mental disorders, and, ultimately, death. As many as 70,000 people are infected in Central and East Africa” (Source).
Another example is hookworm infections in humans. These infections are caused by intestinal worm parasites transmitted by contaminated soil to humans. Hookworm infections can cause internal blood loss and are the leading cause of anemia and protein malnutrition in the world. This is especially prevalent among pregnant women and children. More than half a billion people in Africa, Latin-America, Southeast Asia, and China’s poverty-stricken areas have hookworm infections (Source).
Some other tropical infections caused by parasites include leishmaniasis, lymphatic filariasis, onchocerciasis, and schistosomiasis. However, not all tropical infections are caused by parasites, and some are caused by bacteria. Tropical infections caused by bacteria include Buruli ulcer, trachoma, and yaws.
Neglected diseases are difficult to treat since the population affected by these diseases are often diagnosed in the later stages, which is more difficult to treat. Even if these populations are diagnosed at an earlier stage, most can’t afford the medication used to treat the disease. However, the NIH launched the Therapies for Rare and Neglected Diseases to combat this problem. This program aims to “create an integrated research pipeline to jump-start the development of new treatments for rare and neglected disease.”
National Human Genome Research Institute. "Neglected Diseases FAQ."
Genome.gov, 14 May 2012, www.genome.gov/FAQ/Neglected-Diseases.
Accessed 21 Mar. 2021.
By: Sreenidhi Saripalli
Rebecca Lee Crumpler: First Female African-American Physician
There are many firsts when it comes to medicine, but have you ever wondered who the first African-American female physician in the United States was? In honor of Black history month, today’s blog post will remember the legacy of Rebecca Lee Crumpler, a woman who, despite all odds, succeeded beyond any measure and inspired many to follow her path.
Rebecca Lee Crumpler, born Rebecca Davis in 1831, grew up in Delaware under the care of her aunt. Her aunt was known for providing care for those who were ill, and Rebecca often helped her care for sick neighbors. As a result, Rebecca was influenced to pursue medicine (Source).
Around 1852, Crumpler worked as a nurse for 8 years and then took the bold step of applying to medical school. Crumpler was accepted as one of the 12 females to the New England Female Medical College and earned her medical degree. From its inception, many male physicians denounced the New England Female Medical College. They often complained that women lacked the physical strength required to practice medicine or argued that women were incapable of mastering medical curriculum since the topics taught were inappropriate for their “sensitive and delicate nature.” Fortunately, the founders of the hospital ignored the outrageous claims and organized a school that would provide medical education for females (Source).
In 1864, Rebecca became the first and only graduate of the New England Female Medical College, seeing as the school shut down in 1873. To put Rebecca’s incredible achievement in perspective, in 1860, out of 54,543 physicians in the United States, only 300 were women. None of them were African-American. As late as 1920, there were only 65 African-American woman doctors in the United States (Source).
Throughout her practice, Rebecca Lee Crumpler was subject to unfair racism, rude behavior, and sexism from many people. There were even pharmacists who refused to honor the medications she prescribed to her patients due to the color of Rebecca’s skin and her gender. Yet, Crumpler persevered and went on to publish a book titled “A Book of Medical Discourses in Two Parts” for women and children’s health (Source).
Rebecca Lee Crumpler died in Hyde Park on March 9, 1895. Her story is a bright light to those who aim to follow their passions, regardless of what others think of them. By facing adversity, forging forward, and bringing diversity and passion into her field, Rebecca Lee Crumpler’s legacy will be forever remembered (Source).
Traditional Epidemiology
Traditional epidemiology is the practice of diagnosing illness using traditional and cultural methods. Often in modern epidemiology, the cause of illness is attributed to viruses, bacteria, carcinogens, and pathogens. However, in traditional epidemiology, the cause of illness is attributed to factors such as the evil eye, envy, hate, and jealousy (Spector 9e, 78).
Most commonly in traditional epidemiology, illness is associated with the evil eye. The evil eye is the belief that a person with negative intentions can project harm by staring at the property of another person or the person themself. The evil eye is one of the oldest and most widespread superstition and has roots in numerous countries around the world. While some see the evil eye as superstition, others see it as religion and there are slight variations in the belief across the globe. These variations include how the evil eye is cast, who can cast it, who can receive it, and the degree of the power it has (Spector 9e 78).
But the common beliefs of the evil eye as outlined by Rachel Spector are:
Power comes from the eye or mouth and strikes the victim
The injury is sudden
The person who casts the evil eye may not be aware of this power
The afflicted person may or may not know the source of the evil eye
The injury caused by the evil eye can be reversed with rituals or symbols
This belief helps explain sickness and misfortune (Dundees, 1992; Maloney, 1976,p. Vii; Radford, 2013)
Other agents of disease include soul loss, spirit possession, spells, and hexes, and prevention is a ritual of protecting oneself from these agents.
Illness is also commonly attributed to people who have the ability to make other people ill. Examples are witches and voodoo practitioners, hence the arising of scapegoating. Prevention of this would be to avoid people who represent illness. Other agents to be avoided are envy, hatred, and jealousy.
Traditional practices that are used to protected health are as follows by Rachel Spector:
The use of protective objects
The use of substances that are ingested, eliminated from the diet, and are worn or hung in the home
The practices of religion, which include burning candles and prayer
Spector, Rachel E. Cultural Diversity in Health and Illness. 9th ed., Pearson
Education, 2000.
By: Sreenidhi Saripalli
Traditional Health Restoration Methods Among the Asian Population
There are many ancient forms of restoring one’s health. In this blog post, you will learn about some of the methods used among the Chinese population. Please note that traditional methods vary greatly among people, and not everyone uses these methods. It’s important to recognize that everyone comes from different cultural backgrounds, and generalizations or assumptions must never be made.
First, and arguable the most widespread method of traditional health restoration, is acupuncture.
Acupuncture is a key component of Chinese traditional medicine and is the practice of puncturing the body with a special metal needle to cure disease or relieve pain. Nowadays, it’s increasingly being used for overall wellness, including stress management (Source). The specific points are predetermined for the treatment of specific symptoms and are called meridians. There are also different types of needles for different purposes (Wallnöfer & von Rottauscher, 1972).
Acupuncture is based upon the concept of a fixed network of meridians that extend throughout the body. Since the networks merge and have outlets on the skin, it is believed that internal problems can be treated by puncturing the meridians (Spector 9e, 178). For example, an arrowhead needle is used for superficial pricking, a round needle is used for massaging, a blunt needle is used for knocking or pressing, and a filiform needle is the most extensively used type of needle.
Another well known method of traditional Chinese health restoration is cupping. Cupping involves burning the oxygen out of a small glass to create a vacuum, then placing the glass on the person’s skin. Cupping is used to draw blood and lymph to the surface of a body to increase circulation.
Bleeding is another form of healing. It’s typically done with leeches, and only small amounts of blood are removed. Medicinal herbs were also widely used in Chinese healing. The most prominent herb used is the Ginseng root (Source). Ginseng has numerous beneficial health properties including boosting the immune system, decreasing LDL cholesterol, lowering blood sugar, and improving agility (University of Maryland Medical Center, 2014). A commonly held belief regarding herbs is that herbs gathered at night are more effective. Additionally, the storage and preparation is vital to the release of therapeutic properties.
The Chinese ways of healing are rich in tradition and culture, and it’s important to be appreciative of the cultural aspects associated with healing. These are just some of the many traditional health restoration methods among the Chinese population.
By: Sreenidhi Saripalli
Breast Cancer Disparities
Breast cancer, a cancer that develops in the breasts, is a cancer that can severely affect many people. During breast cancer, breast cells begin to grow abnormally. These cells divide more rapidly than healthy cells do, which causes a massive lump to form. After this process, some obvious symptoms show up, including a newly inverted nipple, redness over the breast, and dimpling of the breast. (source)
Unfortunately, breast cancer is extremely common. During 2009-2013, approximately 221,000 breast cancers were diagnosed annually, and during 2010-2014, approximately 41,000 deaths from breast cancer have occurred annually. While breast cancer affects people of all ethnicities, breast cancer mortality has been proven to be 41% higher among Black women (29.2 deaths per 100,000 population) than white women (20.6 deaths in 100,000 population). Additionally, breast cancer death rates have decreased faster among white women (-1.9% annually) than among Black women (-1.5% annually). (source)
First, a major leading factor for Black people being more susceptible to breast cancer is obesity. Being medically overweight leads to an increased rate in getting diagnosed. Oftentimes, Black people also tend to be racially discriminated against and end up living in more disadvantaged neighborhoods where grocery stores are scarce, and sidewalks are not maintained. These factors limit Black people from maintaining the health they need in order to stay at a healthy weight. (source)
Additionally, Black people are also more likely to get breast cancer because they are likely to reach puberty earlier. Studies have shown that Black girls are 40% more likely than white girls to begin mentustration before age 11. These results have shown to correlate with higher rates of obesity and miscarriage. (source)
Although breast cancer disparities are still a huge problem today, solutions are being provided, and there is hope that things can change! There is so much that YOU can do to help out: increase community awareness; set priorities among disparities to be addressed at the federal, state, tribal, and local levels; advocate many reasons for expending resources; and the list continues. It’s the little things you can do that make a difference.
By: Emily Wang
Editor: Sreenidhi Saripalli
The Immortal Life of Henrietta Lacks by Rebecca Skloot: Book Review
As I was searching for a book to read for my English class, I stumbled upon “The Immortal Life of Henrietta Lacks” by Rebecca Skloot and immediately thought that this is a book all aspiring physicians MUST read. The book brings to light many of the failures of the healthcare system and healthcare research that occurred in the past towards African American patients. It offers many valuable lessons that need to be considered when interacting with patients in healthcare.
The Immortal Life of Henrietta Lacks is centered around a 30-year-old African American woman named Henrietta Lacks. Henrietta was diagnosed with cervical cancer at Johns Hopkins Hospital in 1951, a period of segregation. At the time, it wasn’t unusual to give patients’ tissue samples and cells to researchers, and Henrietta’s cells were given to Dr. Gey to research growing human cells outside of the body. After Henrietta’s cancer cells proved successful in surviving and dividing outside of her body, they were labeled HeLa after the initials of her first and last name. HeLa cells were an integral part of biomedical research, with the cells seeing hundreds of labs around the world. Despite this, the Lacks family initially didn’t know that technically a part of Henrietta was still alive. They never received any financial compensation and had limited access to health care as a result of their poverty (Source).
One of the largest issues “The Immortal Life of Henrietta Lacks” touches on is informed consent.
Informed consent is defined as “a process for enabling individuals to make voluntary decisions about participating in research with an understanding of the purpose, procedures, risks, benefits, and alternatives. Informed consent is premised on well-established ethical principles, including respect for persons, beneficence, and justice” (Source).
When Henrietta was in the middle of radiation treatment for cervical cancer, she was not aware that the treatments would leave her infertile. Although medical records marked that Henrietta was aware that she would be infertile, nearly halfway through treatment she asked a doctor when she could have her next child. Henrietta was also never informed of her cells being used for research. Although Henrietta passed away before HeLa became widespread, her family was also in the dark about Henrietta’s cells being alive. The Lacks family’s unawareness of the implications of Henrietta’s treatment and her cells being used for research led to many hardships down the road for the family. The family’s lack of knowledge of cell research and scientific terminology only exacerbated the situation.
Overall, reading Rebecca Skloot’s “The Immortal Life of Henrietta Lacks” emphasized the need for a strong patient-provider relationship with a foundation of trust. It also encourages a discussion of ethics in medicine and medical research, and the book forces the reader to think about the impact of the choices certain people made on Henrietta Lacks and her family.
By: Sreenidhi Saripalli
Lung Cancer Disparities Among the Black Community
As many of you may know, lung cancer is a common disease that can affect different people. According to healthline.com, lung cancer is the second most common cancer in the United States, with an estimated 228,820 new cases each year and roughly 135,720 deaths occurring from it. However, while lung cancer can affect people of all different races and ethnicities, certain populations are more susceptible to cancer than others.
Significantly for African Americans, lung cancer is developed at a higher rate than any other racial or ethnic group in the country. Unfortunately, Black Americans are 37% more likely to develop lung cancer than their white counterparts while also facing lower survival rates. According to the CDC, a substantial proportion of the adult population with insufficient resources is vulnerable to health problems. What’s more, those who recognize that they have lung cancer are, on average, diagnosed at a more severe stage than white patients. Often, by the time black patients get diagnosed, cancer has spread to more organs in the body, making their condition harder to treat. (source)
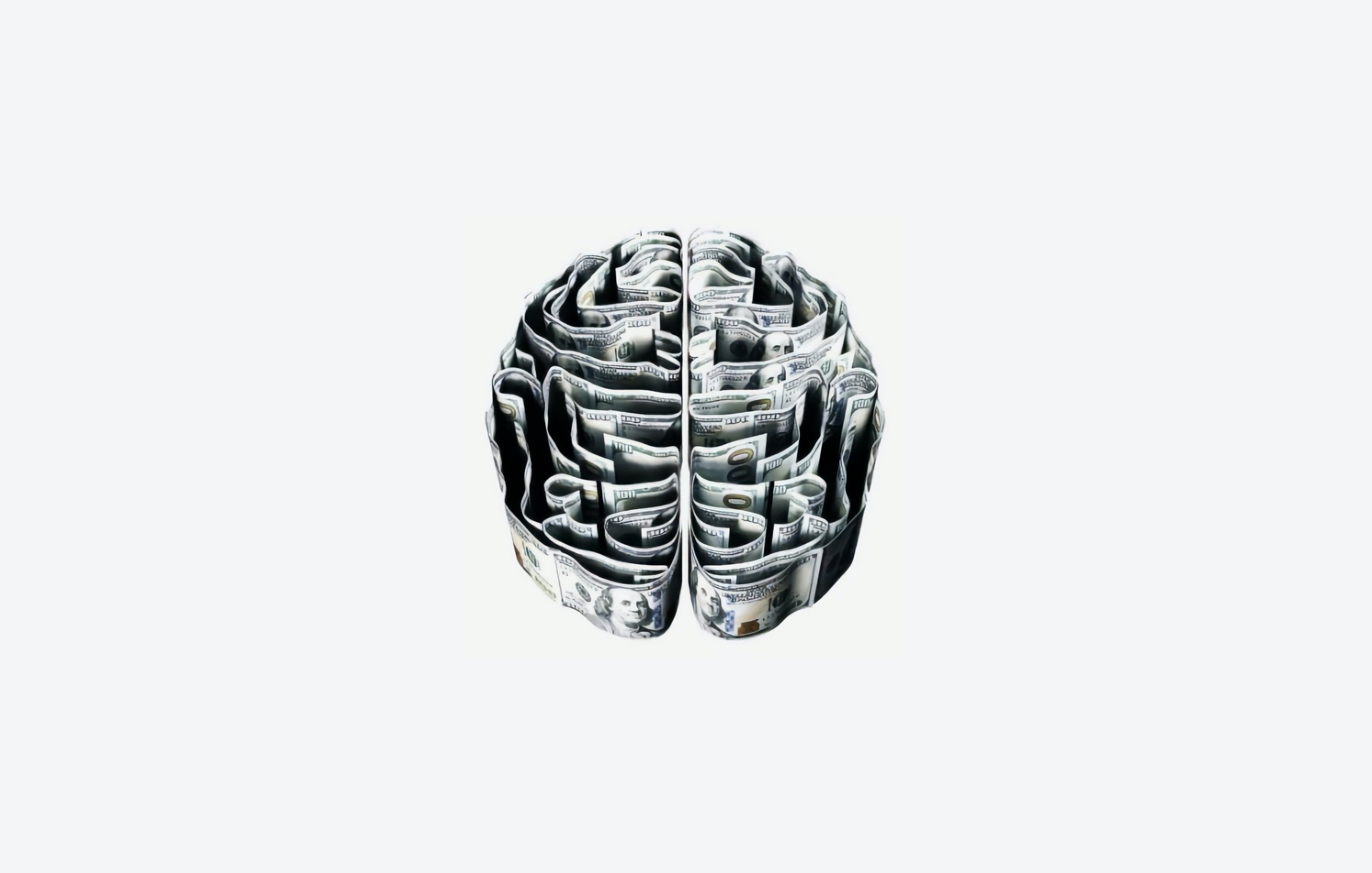
First, a major leading factor for Black people being more susceptible to lung cancer is education and income inequality. The racial/ethnic disparity in both income and education has been reported to be the lowest for non-Hispanic mixed races and Asian/Pacific Islanders and intermediate for non-Hispanic blacks. The CDC has reported that people who are low income and face socioeconomic circumstances are not only in short of adequate access to healthcare, but also have a greater risk of mortality, morbidity, and higher chances of doing risky behavior, specifically not completing high school. Studies have shown that people who did not complete high school were twice as likely to have disabilities as those who did complete high school, and the proportion of people with disabilities living below the poverty level was over two times that of people without disabilities. (source)
Additionally, since Black Americans often live in low socioeconomic circumstances, they often do not have the same high-quality healthcare as people of other races and ethnicities. Under these conditions, healthcare treatment is not easily affordable to many people of the Black community. Some healthcare treatments that African Americans lack include cancer screening and testing. Without these resources, Black people are 66% far less likely to be put on a path with newer, targeted therapies that lead to longer living lives. (source)
Finally, more Black people than people of any other race live in unhealthy housing units. Although the proportion of unhealthy housing units had decreased from 2007 to 2009, the disparity is still substantial, with Non-Hispanic black people having the highest percentage of householders living in inadequate, unhealthy housing (source). Characteristics of unhealthy housing include lack of structural and safety features and poor indoor air quality. A lack of structural and safety features can cause an increase in the risk of injury and higher blood levels. Poor air quality can lead to cancers, cardiovascular disease, and asthma. Under these conditions, there are huge gaps between the healthiest people and those who are unhealthy.
Although lung cancer disparities are still a huge problem today, solutions are being provided, and there is hope that things can change! For people who face income and education inequality, the US Department of Education, Institute of Education Sciences, has identified effective ways to lower school dropout rates. Additionally, The US Task Force on Community Preventive Services has recommended useful methods to promote healthy and safe spaces for families of low income and methods to stop risk-taking behaviors among adolescents. For people who do not have the best access to healthcare, partnering with community leaders and health organizers can best help people to understand and address the disparities faced by vulnerable communities. For people facing inadequate and unhealthy housing problems, the Surgeon General’s Call to Action to Promote Healthy Homes has recommended many useful interventions to prevent home hazards, including improving ventilation, avoiding wastewater systems to dispose of toxic chemicals, and using integrated pest management. With this in mind, there is also so much that YOU can do: increase community awareness, set priorities among disparities to be addressed at the federal, state, tribal, and local levels, advocate many reasons for expending resources, and the list continues. It’s the little things you can do that make a difference.